Fast Lab Solutions
Case Study
Heart Failure in the GP practice

How to quickly reach a diagnosis with the determination of NT-proBNP from capillary blood
Dyspnoea is a common symptom in GP practices. Dr. Stefan Bauernschmitt is an internist, sports and emergency physician and runs the GP group practice “med. in” with his colleagues Dr. Franz Macht and Dr. Maria Sarawara in several locations throughout Bavaria (Pottenstein, Betzenstein and Gößweinstein). At all three practice locations, NT-proBNP is determined with the LumiraDx Platform when patients present with corresponding symptoms. In this interview, Dr. Bauernschmitt answers questions about the guidelines and effective procedures for the diagnosis of suspected heart failure (HF).

Dr. Bauernschmitt, in addition to your in-house laboratory analyzer, you also use the LumiraDx Platform for the point-of-care determination of laboratory biomarkers. How do you measure the NT-proBNP value in patients with suspected heart failure?
Natriuretic peptides are an essential component in the differential diagnosis of shortness of breath. Its determination is recommended in clinical guidelines and has been standard practice for many years. In our practices, we measure the NT-proBNP values of patients with suspected heart failure directly from capillary blood taken from the fingertip using the LumiraDx Platform. This enables us to reach a suspected diagnosis very quickly and efficiently and we are then able to discuss the result with our patients in the same appointment. The fact that we can now also test directly from capillary blood with this modern technology makes the procedure efficient and easier to delegate to other members of the team.

In view of the clinical guidelines, how should you proceed in patients with suspected heart failure in the GP practice?
The approach in GP practices is very clear and established. The clinical guidelines recommend that three important pillars are covered. It starts with the medical history and clinical examination. The classic symptoms of heart failure are, for example, water retention in the legs and shortness of breath on exertion. Then a resting ECG is taken, and thirdly blood is taken to determine the natriuretic peptides. If either the ECG or the NT-proBNP are abnormal, further examinations are required to confirm the suspicion of heart failure. Of course, this is particularly important if both the ECG and the NT-proBNP are abnormal. These pillars – medical history, clinical examination, resting ECG and NT-proBNP – are the guiding principles for us in GP practice.
Figure 1: NT-proBNP cut-offs
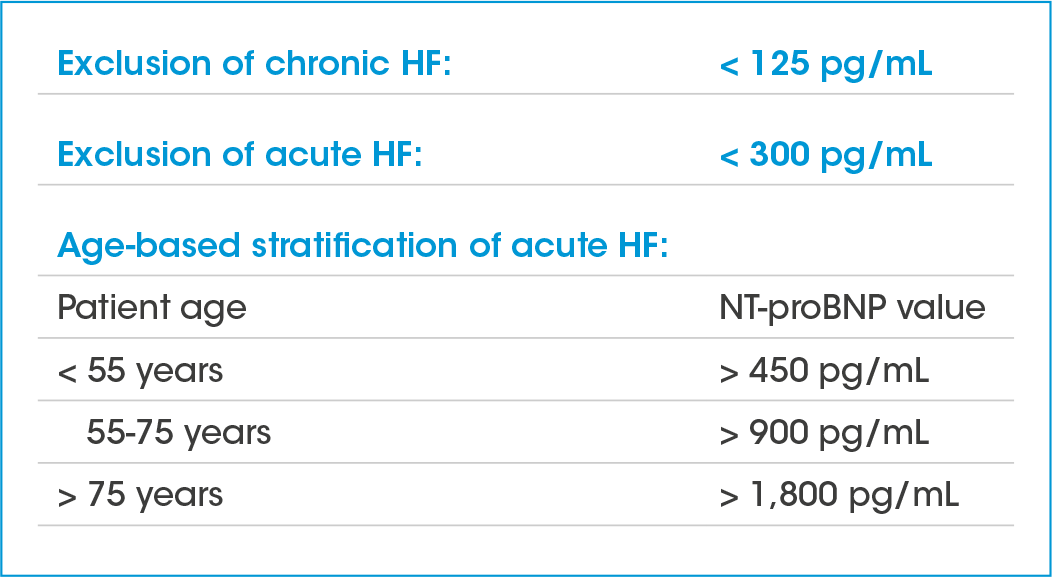
Fig.1 modified from European Society of Cardiology (ESC) Pocket Guidelines “Acute and Chronic Heart Failure”, German Cardiac Society (DGK), version 2021
What must be considered with regards to the cut-off values for NT-proBNP?
Basically, it can first be said that a single cut-off value for NT-proBNP does not provide optimal predictive values, but that the overall clinical picture must always be taken into account. The biomarker NT-proBNP has been a proven tool for the diagnosis of acute and chronic heart failure for many years. As with any laboratory parameter, the NT-proBNP cut-off values should always be considered when routinely using the test for clinical decisions. It is also advisable to provide information describing the procedure and the cut-off values. If the NT-proBNP value is lower than 125 pg/mL and the patient has been short of breath for weeks or longer, chronic heart failure is unlikely.
Acute heart failure is unlikely if the patient has had shortness of breath for a few hours and the NT-proBNP is lower than 300 pg/mL. Age also has a relevant influence on the threshold values. In their pocket guidelines, the cardiology societies have listed age-related NT-proBNP thresholds for the acute scenario, which, if exceeded, are highly likely to indicate acute heart failure (Fig. 1).1
How do you further proceed if you have a suspected diagnosis of heart failure based on an abnormal resting ECG and/or an elevated NT-proBNP value?
It is important to us that the suspected diagnosis is first discussed with the patient. We then look at the overall clinical examination and assessment. For example, if a patient has significant shortness of breath and an NT-proBNP value of over 300 or 400 pg/mL, then acute heart failure could be a relevant possibility considering the symptoms. In our practices at “med. in”, we then have the option of using echocardiography to obtain information about the disease with regards to the site of occurrence (left heart, right heart or global heart failure) and the cause of the functional disorder (reduced Ejection Fraction/ HFrEF or preserved Ejection Fraction/ HFpEF). Depending on the results, this enables us to initiate medical drug therapy immediately if necessary. This is an advantage, as we know that starting treatment for heart failure at an early stage can alleviate symptoms and delay the progression of the disease. If necessary, we refer the patient to a cardiologist for further clinical diagnostics.
You also treat patients with diabetes in your practice. To what extent do you take their risk profile for cardiovascular disease into account?
Patients with diabetes must always be closely monitored. This includes, among other things, carrying out preventive examinations with a view to secondary diseases. Diabetes mellitus is an important comorbidity in patients with heart failure. The 2023 ESC guidelines for the management of cardiovascular disease in patients with diabetes describe the increased risk of patients with type 2 diabetes for cardiovascular diseases, such as coronary heart disease or heart failure. Determination of NT-proBNP is recommended in cases of suspected heart failure and/ or abnormal ECGs.2 This means that the pumping function of the heart is now also coming into focus with the aim of administering potent medication at an early stage to improve the prognosis. SGLT-2 inhibitors, some of which can be used as cross-diagnostic drugs for the treatment of type 2 diabetes mellitus as well as chronic heart failure and kidney failure, are proving to be helpful here and have shown clear benefits for patient outcomes.
You run your own lab in your practice with a laboratory analyzer. Why do you also determine a number of parameters, such as NT-proBNP, directly on the patient using the LumiraDx point-of-care system?
Determining biomarkers directly on the patient has advantages for us. The ability to test patient samples with just a drop of blood from the fingertip has proven to be a very convenient and modern solution for both us and our patients. In particular, we notice improved time efficiency and better communication with our patients. Testing with a point-of-care system allows us to make quick clinical decisions that we can discuss immediately with our patients and from which a therapeutic decision or further diagnostics can be derived immediately. With our approach, we help to minimize referrals to cardiology specialists with long waiting times and recurring hospital admissions. There are associated cost savings for the healthcare system by initiating therapy at an early stage. We have also checked the quality of the technology and can therefore be sure that the accuracy of the results are reliable.
References:
1. European Society of Cardiology (ESC) Pocket Guidelines “Acute and Chronic Heart Failure”, German Cardiac Society (DGK), version 2021
2. European Society of Cardiology (ESC) Guidelines for the management of cardiovascular disease in patients with diabetes, European Heart Journal (2023) 44, 4043–4140
The interview was conducted by Stephanie Neemann, LumiraDx; Copyright photos LumiraDx and Dr. med. Stefan Bauernschmitt
The information is of an advisory nature and does not claim to be complete. Neither the authors nor LumiraDx are liable in any way for the diagnosis made by the physician and the prescribed therapy. For more information, see lumiradx.com or email LumiraDx customer service at customerservices@lumiradx.com.
This document and its contents are copyright LumiraDx Group Limited © 2024. All rights reserved worldwide. The information is subject to change without notice.
LumiraDx UK Ltd (Registration Number: 09206123), Unit 1, Block 5, Dumyat Business Park, Bond Street, Alloa, FK10 2PB, UK
BetterHealthExperiencesOutcomes
Supporting healthier lives, for individuals, communities and wider society.
Enabling responsive, personal relationships between patients and care teams.
Controlling and reducing costs to help ease pressure on healthcare budgets.